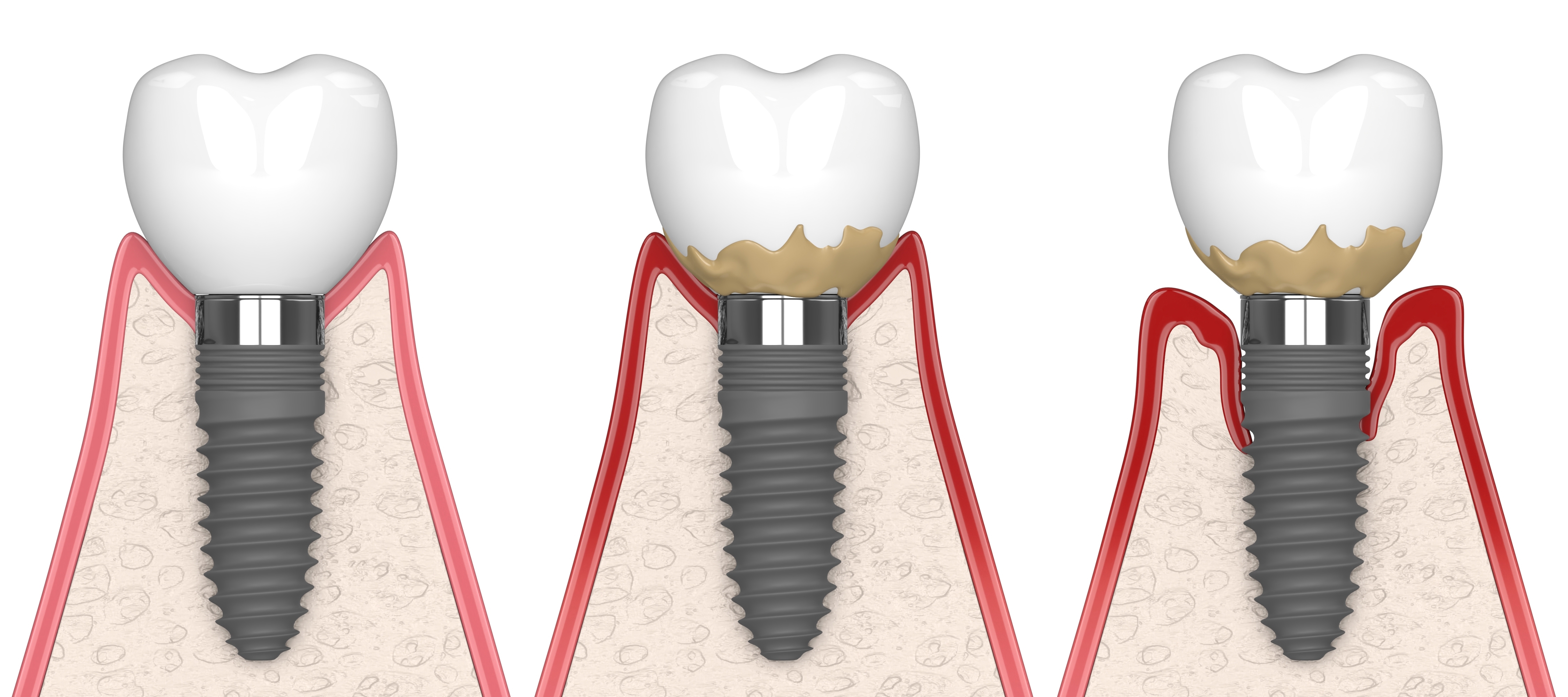
Peri-implantitis is a condition characterized by inflammation and infection around dental implants, which can lead to bone loss and implant failure if left untreated. The treatment of peri-implantitis typically involves a combination of mechanical and antimicrobial therapies and may also involve regenerative procedures to rebuild lost bone and tissue. Here are some of the various methods that may be used in the treatment of dental peri-implantitis:
Mechanical Debridement: This involves the removal of plaque and calculus from the implant surface using hand instruments or ultrasonic scalers. Mechanical debridement is typically the first step in the treatment of peri-implantitis and can be effective in removing bacterial biofilm.
Antimicrobial Therapy: Antibiotics, antiseptics, and disinfectants may be used to help eliminate bacteria that have colonized the implant surface. Topical antimicrobials, such as chlorhexidine, may be applied directly to the implant surface or used as a mouth rinse.
Surgical Therapy: If the infection and inflammation have progressed to a more advanced stage, surgical therapy may be necessary. This may involve the removal of damaged tissue, the placement of bone grafts or tissue regeneration materials, and the use of barrier membranes to encourage new tissue growth.
Maintenance Therapy: the peri-implantitis has been treated, ongoing maintenance therapy is critical to prevent recurrence of the infection. This may involve regular follow-up appointments, professional cleanings, and the use of antimicrobial agents.
In summary, the treatment of dental peri-implantitis typically involves a combination of mechanical and antimicrobial therapies and may also involve regenerative procedures in more advanced cases. The most effective treatment plan will depend on the severity and stage of the peri-implantitis, as well as other factors such as the patient's overall health and oral hygiene practices.

Book Appointment